| 1. |
Wu Z, Xia F, Wang W, et al. Worldwide burden of liver cancer across childhood and adolescence, 2000–2021: a systematic analysis of the Global Burden of Disease Study 2021. EClinicalMedicine, 2024, 75: 102765. doi: 10.1016/j.eclinm.2024.102765.
|
| 2. |
Younossi ZM, Kalligeros M, Henry L. Epidemiology of metabolic dysfunction-associated steatotic liver disease. Clin Mol Hepatol, 2024 Aug 19. doi: 10.3350/cmh.2024.0431. Online ahead of print.
|
| 3. |
Wang R. Two’s company, three’s a crowd: can H2S be the third endogenous gaseous transmitter?. FASEB J, 2002, 16(13): 1792-1798.
|
| 4. |
Wallace JL, Wang R. Hydrogen sulfide-based therapeutics: exploiting a unique but ubiquitous gasotransmitter. Nat Rev Drug Discov, 2015, 14(5): 329-345.
|
| 5. |
Munteanu C, Turnea MA, Rotariu M. Hydrogen sulfide: An emerging regulator of oxidative stress and cellular homeostasis—A comprehensive one-year review. Antioxidants (Basel), 2023, 12(9): 1737. doi: 10.3390/antiox12091737.
|
| 6. |
Pandey T, Pandey V. Hydrogen sulfide (H2S) metabolism: Unraveling cellular regulation, disease implications, and therapeutic prospects for precision medicine. Nitric Oxide, 2024, 144: 20-28.
|
| 7. |
Sun HJ, Wu ZY, Nie XW, et al. Implications of hydrogen sulfide in liver pathophysiology: Mechanistic insights and therapeutic potential. J Adv Res, 2020, 27: 127-135.
|
| 8. |
Nguyen TTP, Nguyen PL, Park SH, et al. Hydrogen sulfide and liver health: Insights into liver diseases. Antioxid Redox Signal, 2024, 40(1-3): 122-144.
|
| 9. |
徐文静. 肝脏内源性硫化氢代谢和功能. 生命的化学, 2020, 40(8): 1289-1297.
|
| 10. |
Jeitner TM, Azcona JA, Ables GP, et al. Cystine rather than cysteine is the preferred substrate for β-elimination by cystathionine γ-lyase: implications for dietary methionine restriction. Geroscience, 2024, 46(4): 3617-3634.
|
| 11. |
Kabil O, Vitvitsky V, Xie P, et al. The quantitative significance of the transsulfuration enzymes for H2S production in murine tissues. Antioxid Redox Signal, 2011, 15(2): 363-372.
|
| 12. |
Kabil O, Banerjee R. Enzymology of H2S biogenesis, decay and signaling. Antioxid Redox Signal, 2014, 20(5): 770-782.
|
| 13. |
Hao Y, Hao Z, Zeng X, et al. Gut microbiota and metabolites of cirrhotic portal hypertension: a novel target on the therapeutic regulation. J Gastroenterol, 2024, 59(9): 788-797.
|
| 14. |
Li X, Jiang K, Ruan Y, et al. Hydrogen sulfide and its donors: Keys to unlock the chains of nonalcoholic fatty liver disease. Int J Mol Sci, 2022, 23(20): 12202. doi: 10.3390/ijms232012202.
|
| 15. |
Sun X, Wu S, Mao C, et al. Therapeutic potential of hydrogen sulfide in ischemia and reperfusion injury. Biomolecules, 2024, 14(7): 740. doi: 10.3390/biom14070740.
|
| 16. |
Lin X, Zhou Y, Ye L, et al. A bibliometric and visualized analysis of hepatic ischemia-reperfusion injury (HIRI) from 2002 to 2021. Heliyon, 2023, 9(11): e22644. doi: 10.1016/j.heliyon.2023.e22644.
|
| 17. |
Yang F, Gao H, Niu Z, et al. Puerarin protects the fatty liver from ischemia-reperfusion injury by regulating the PI3K/AKT signaling pathway. Braz J Med Biol Res, 2024, 57: e13229. doi: 10.1590/1414-431X2024e13229.
|
| 18. |
Dugbartey GJ. Cellular and molecular mechanisms of cell damage and cell death in ischemia-reperfusion injury in organ transplantation. Mol Biol Rep, 2024, 51(1): 473. doi: 10.1007/s11033-024-09261-7.
|
| 19. |
Tang SP, Mao XL, Chen YH, et al. Reactive oxygen species induce fatty liver and ischemia-reperfusion injury by promoting inflammation and cell death. Front Immunol, 2022, 13: 870239. doi: 10.3389/fimmu.2022.870239.
|
| 20. |
Press AT, Ungelenk L, Medyukhina A, et al. Sodium thiosulfate refuels the hepatic antioxidant pool reducing ischemia-reperfusion-induced liver injury. Free Radic Biol Med, 2023, 204: 151-160.
|
| 21. |
Zhao S, Song T, Gu Y, et al. Hydrogen sulfide alleviates liver injury through the S-sulfhydrated-kelch-like ECH-associated protein 1/nuclear erythroid 2-related factor 2/low-density lipoprotein receptor-related protein 1 pathway. Hepatology, 2021, 73(1): 282-302.
|
| 22. |
Bos EM, Snijder PM, Jekel H, et al. Beneficial effects of gaseous hydrogen sulfide in hepatic ischemia/reperfusion injury. Transpl Int, 2012, 25(8): 897-908.
|
| 23. |
Ruan Z, Liang M, Deng X, et al. Exogenous hydrogen sulfide protects fatty liver against ischemia-reperfusion injury by regulating endoplasmic reticulum stress-induced autophagy in macrophage through mediating the class A scavenger receptor pathway in rats. Cell Biol Int, 2020, 44(1): 306-316.
|
| 24. |
Cheng P, Wang F, Chen K, et al. Hydrogen sulfide ameliorates ischemia/reperfusion-induced hepatitis by inhibiting apoptosis and autophagy pathways. Mediators Inflamm, 2014, 2014: 935251. doi: 10.1155/2014/935251.
|
| 25. |
Wu D, Wang H, Teng T, et al. Hydrogen sulfide and autophagy: A double edged sword. Pharmacol Res, 2018, 131: 120-127.
|
| 26. |
Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology, 2023, 78(6): 1966-1986.
|
| 27. |
Peh MT, Anwar AB, Ng DS, et al. Effect of feeding a high fat diet on hydrogen sulfide (H2S) metabolism in the mouse. Nitric Oxide, 2014, 41: 138-145.
|
| 28. |
Xu W, Cui C, Cui C, et al. Hepatocellular cystathionine γ lyase/hydrogen sulfide attenuates nonalcoholic fatty liver disease by activating farnesoid X receptor. Hepatology, 2022, 76(6): 1794-1810.
|
| 29. |
Li M, Xu C, Shi J, et al. Fatty acids promote fatty liver disease via the dysregulation of 3-mercaptopyruvate sulfurtransferase/hydrogen sulfide pathway. Gut, 2018, 67(12): 2169-2180.
|
| 30. |
Sun L, Zhang S, Yu C, et al. Hydrogen sulfide reduces serum triglyceride by activating liver autophagy via the AMPK-mTOR pathway. Am J Physiol Endocrinol Metab, 2015, 309(11): E925-E935. doi: 10.1152/ajpendo.00294.2015.
|
| 31. |
Wu D, Zhong P, Wang Y, et al. Hydrogen sulfide attenuates high-fat diet-induced non-alcoholic fatty liver disease by inhibiting apoptosis and promoting autophagy via reactive oxygen species/phosphatidylinositol 3-kinase/AKT/mammalian target of rapamycin signaling pathway. Front Pharmacol, 2020, 11: 585860. doi: 10.3389/fphar.2020.585860.
|
| 32. |
Grewal T, Buechler C. Emerging insights on the diverse roles of proprotein convertase subtilisin/kexin type 9 (PCSK9) in chronic liver diseases: Cholesterol metabolism and beyond. Int J Mol Sci, 2022, 23(3): 1070. doi: 10.3390/ijms23031070.
|
| 33. |
Cui X, Yao M, Feng Y, et al. Exogenous hydrogen sulfide alleviates hepatic endoplasmic reticulum stress via SIRT1/FoxO1/PCSK9 pathway in NAFLD. FASEB J, 2023, 37(8): e23027. doi: 10.1096/fj.202201705RR.
|
| 34. |
Ci L, Yang X, Gu X, et al. Cystathionine γ-lyase deficiency exacerbates CCl4-induced acute hepatitis and fibrosis in the mouse liver. Antioxid Redox Signal, 2017, 27(3): 133-149.
|
| 35. |
Zhang F, Jin H, Wu L, et al. Diallyl trisulfide suppresses oxidative stress-induced activation of hepatic stellate cells through production of hydrogen sulfide. Oxid Med Cell Longev, 2017, 2017: 1406726. doi: 10.1155/2017/1406726.
|
| 36. |
Damba T, Zhang M, Buist-Homan M, et al. Hydrogen sulfide stimulates activation of hepatic stellate cells through increased cellular bio-energetics. Nitric Oxide, 2019, 92: 26-33.
|
| 37. |
杜少严, 尹硕, 郝文洋, 等. 硫化氢在肝脏疾病中的研究进展. 临床荟萃, 2019, 34(12): 1127-1130.
|
| 38. |
Lu G, Zhang Y, Ren Y, et al. Diversity and comparison of intestinal desulfovibrio in patients with liver cirrhosis and healthy people. Microorganisms, 2023, 11(2): 276. doi: 10.3390/microorganisms11020276.
|
| 39. |
郝运, 李川, 文天夫, 等. 全球及中国的肝癌流行病学特征: 基于《2022全球癌症统计报告》解读. 中国普外基础与临床杂志, 2024, 31(7): 781-789.
|
| 40. |
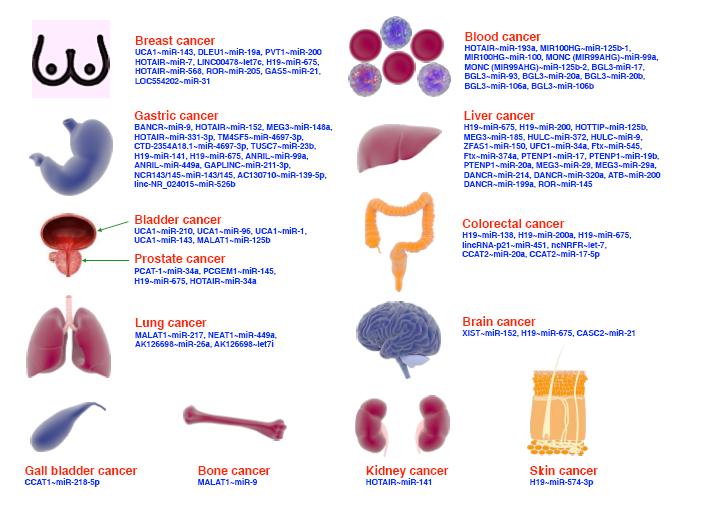
Oza PP, Kashfi K. The triple crown: NO, CO, and H2S in cancer cell biology. Pharmacol Ther, 2023, 249: 108502. doi: 10.1016/j.pharmthera.2023.108502.
|
| 41. |
Lu S, Gao Y, Huang X, et al. GYY4137, a hydrogen sulfide (H₂S) donor, shows potent anti-hepatocellular carcinoma activity through blocking the STAT3 pathway. Int J Oncol, 2014, 44(4): 1259-1267.
|
| 42. |
Pan Y, Ye S, Yuan D, et al. Hydrogen sulfide (H2S)/cystathionine γ-lyase (CSE) pathway contributes to the proliferation of hepatoma cells. Mutat Res, 2014, 763-764: 10-18.
|
| 43. |
Zhou YF, Song SS, Tian MX, et al. Cystathionine β-synthase mediated PRRX2/IL-6/STAT3 inactivation suppresses Tregs infiltration and induces apoptosis to inhibit HCC carcinogenesis. J Immunother Cancer, 2021, 9(8): e003031. doi: 10.1136/jitc-2021-003031.
|
| 44. |
Li M, Song X, Jin Q, et al. 3-mercaptopyruvate sulfurtransferase represses tumour progression and predicts prognosis in hepatocellular carcinoma. Liver Int, 2022, 42(5): 1173-1184.
|
| 45. |
Wang SS, Chen YH, Chen N, et al. Hydrogen sulfide promotes autophagy of hepatocellular carcinoma cells through the PI3K/Akt/mTOR signaling pathway. Cell Death Dis, 2017, 8(3): e2688. doi: 10.1038/cddis.2017.18.
|
| 46. |
Wu D, Li M, Tian W, et al. Hydrogen sulfide acts as a double-edged sword in human hepatocellular carcinoma cells through EGFR/ERK/MMP-2 and PTEN/AKT signaling pathways. Sci Rep, 2017, 7(1): 5134. doi: 10.1038/s41598-017-05457-z.
|
| 47. |
Yu M, Yu H, Wang H, et al. Tumor-associated macrophages activated in the tumor environment of hepatocellular carcinoma: Characterization and treatment (Review). Int J Oncol, 2024, 65(4): 100. doi: 10.3892/ijo.2024.5688.
|
| 48. |
He Z, Zhu Y, Ma H, et al. Hydrogen sulfide regulates macrophage polarization and necroptosis to accelerate diabetic skin wound healing. Int Immunopharmacol, 2024, 132: 111990. doi: 10.1016/j.intimp.2024.111990.
|
| 49. |
Ito T, Naini BV, Markovic D, et al. Ischemia-reperfusion injury and its relationship with early allograft dysfunction in liver transplant patients. Am J Transplant, 2021, 21(2): 614-625.
|
| 50. |
Guo Z, Zhao Q, Jia Z, et al. A randomized-controlled trial of ischemia-free liver transplantation for end-stage liver disease. J Hepatol, 2023, 79(2): 394-402.
|
| 51. |
Wang S, Lin X, Tang Y, et al. Ischemia-free liver transplantation improves the prognosis of recipients using functionally marginal liver grafts. Clin Mol Hepatol, 2024, 30(3): 421-435.
|
| 52. |
McLean ST, Holkup S, Tchir A, et al. UW supplementation with AP39 improves liver viability following static cold storage. Res Sq, 2024 Jun 11: rs. 3. rs-4487319. doi: 10.21203/rs.3.rs-4487319/v1.
|
| 53. |
Zhang MY, Dugbartey GJ, Juriasingani S, et al. Sodium thiosulfate-supplemented UW solution protects renal grafts against prolonged cold ischemia-reperfusion injury in a murine model of syngeneic kidney transplantation. Biomed Pharmacother, 2022, 145: 112435. doi: 10.1016/j.biopha.2021.112435.
|
| 54. |
Balaban CL, Rodríguez JV, Tiribelli C, et al. The effect of a hydrogen sulfide releasing molecule (Na2S) on the cold storage of livers from cardiac dead donor rats. A study in an ex vivo model. Cryobiology, 2015, 71(1): 24-32.
|
| 55. |
Dugbartey GJ, Juriasingani S, Zhang MY, et al. H2S donor molecules against cold ischemia-reperfusion injury in preclinical models of solid organ transplantation. Pharmacol Res, 2021, 172: 105842. doi: 10.1016/j.phrs.2021.105842.
|
| 56. |
Zapolski T, Kornecki W, Jaroszyński A. The influence of balneotherapy using salty sulfide-hydrogen sulfide water on selected markers of the cardiovascular system: A prospective study. J Clin Med, 2024, 13(12): 3526. doi: 10.3390/jcm13123526.
|
| 57. |
申欣欣, 张奕华, 黄张建. 硫化氢供体分子研究进展. 中国药科大学学报, 2019, 50(3): 265-273.
|
| 58. |
Ghaffari-Bohlouli P, Jafari H, Okoro OV, et al. Gas therapy: Generating, delivery, and biomedical applications. Small Methods, 2024, 8(8): e2301349. doi: 10.1002/smtd.202301349.
|
| 59. |
Fu J, Mao Y, Han J, et al. A nitric oxide and hydrogen sulfide dual-donating nanosystem for highly synergistic gas-radiotherapy against hepatocellular carcinoma. Biomater Adv, 2023, 144: 213209. doi: 10.1016/j.bioadv.2022.213209.
|
| 60. |
Liu Y, Wang X, Li Z, et al. Cascading detection of hydrogen sulfide and N-acetyltransferase 2 in hepatocellular carcinoma cells using a two-photon fluorescent probe. Anal Chem, 2024, 96(18): 7005-7013.
|